Diabetes Across the Lifespan: Facilitating Healthy Eating for the Whole Family
Published January 2021 | Back to all news and updates
One of the most important strategies for diabetes management and improvement is through maintaining a healthy diet. Combined with physical activity, this can be the pathway to controlling this disease and improving health outcomes.1 Good nutrition is not only important for individuals currently diagnosed with diabetes, but it can be vital for preventing the disease, especially for those who may be predisposed to it, such as family members.2
Nevertheless, making changes to one’s diet is often easier said than done and can be intensified when there are children and a family to support. Factors that can make these lifestyle changes difficult include the affordability of nutritious foods versus cheaper unhealthy foods, the challenge of changing deep-seated habits and beliefs around food,3 and merely being able to access healthy foods, especially for those living in remote areas or low-income urban neighborhoods.4
Community health centers (CHCs) are a source of vital health services for millions of patients, and they have historically been viewed as trusted beacons of information for the vulnerable communities they serve. This positions CHCs to be impactful messengers when it comes to delivering health education, especially for chronic diseases such as diabetes, which many are already engaged in. However, health education alone will not guarantee better health outcomes. Rather, it is the implementation of this health education that is especially important in order to translate what is learned into action. This article will discuss some of these challenges and present innovative solutions from CHCs that aim to facilitate and promote healthy eating for diabetic patients and their families.
Adopting Healthy Eating Practices
One’s culture around food and cooking is often very personal, and habits around nutrition can be difficult to adjust. These habits are built over a lifetime and often span generations, especially from different cultural backgrounds and different countries. Changing one’s approach to nutrition is equally personal and presents an added challenge. Patients may have certain ideas around the appropriate ways to prepare certain foods and what aspects create a complete diet, even if these ideas have been shown to be unhealthy for diabetic patients or those at risk of diabetes.
It is exceedingly important to practice cultural humility when providing nutrition education and encouraging new practices. It is unrealistic to expect patients to fully change this lifetime of habits overnight, and the focus should be on progressively making small changes within the context of their current perspective on nutrition.
Example: One great solution is to conduct food preparation or cooking demonstrations from someone who shares your patients’ background to show how to prepare common dishes in a healthier way.
Availability of Nutritious Food
In order to pursue changes to one’s diet, there has to be a convenient opportunity to obtain the desired food, which is increasingly challenging in many environments. Large grocery stores, produce markets, and farmer’s markets are the best options to access nutritious food such as fresh produce. However, those in very remote settings may live far from grocery stores and not have access to readily available transportation. Additionally, many urban environments, especially in historically low-income neighborhoods, exist in what are considered food deserts5, often without a single option for fresh, healthy food. By acknowledging these barriers, health centers can seek new solutions to facilitate your diabetic patients’ access to healthy food, which will increase the successful implementation of your health education efforts.
Example: Some health centers have implemented transportation solutions that not only serve the patients’ health appointments but include vital social needs, such as trips to the grocery store.
Affordability of Healthy Food
Unfortunately, the healthiest foods are often the more expensive options. Fresh, organic produce and meat-free of chemicals and preservatives are sold at higher prices, often beyond the budget of low-income families. Meanwhile, high-calorie unhealthy foods are cheap and readily available, making it easy to make the decision to prioritize battling the immediate concerns of hunger and financial security over long-term nutrition. When non-nutritious snack food and fast food restaurants are the most affordable and accessible, the nutrition education you deliver to your diabetic patients and their families can be even more challenging to put into practice.
Example: Some health centers have been able to establish a food pantry, partnering with local food banks or volunteers to have free, healthy foods available to patients that need it most.
Innovative Practices to Encourage Healthy Eating6
ArCare – Augusta, AR
After identifying large numbers of diabetic patients who were unable to afford or access healthy foods, ArCare partnered with a local city council to establish The Warehouse – a community site for food storage and distribution. The local university helped acquire grants to pay for important supplies and appliances, and ArCare’s membership within the local food bank allows The Warehouse to be stocked with nutritious food.
Food is distributed monthly to anyone, regardless of diagnosis or income status. On these distribution days, ArCare also provides health screenings, counseling and health education related to chronic diseases, and flu shots in the fall. Local partners are also invited to provide free services, such as cooking demonstrations, education on safe handling and storage, and information and resources around access to the Supplemental Nutrition Assistance Program (SNAP).
Mountain Park Health Center – Phoenix, AZ
Mountain Park Health Center has a well-established diabetes self-management program providing hands-on education around diabetes management. They also offer health education to others in the family, including a program for weight management specifically for pediatric patients and their families. In order to facilitate access to healthy foods, Mountain Park collaborated with local farmers to establish farmers’ markets at two of their clinic sites.
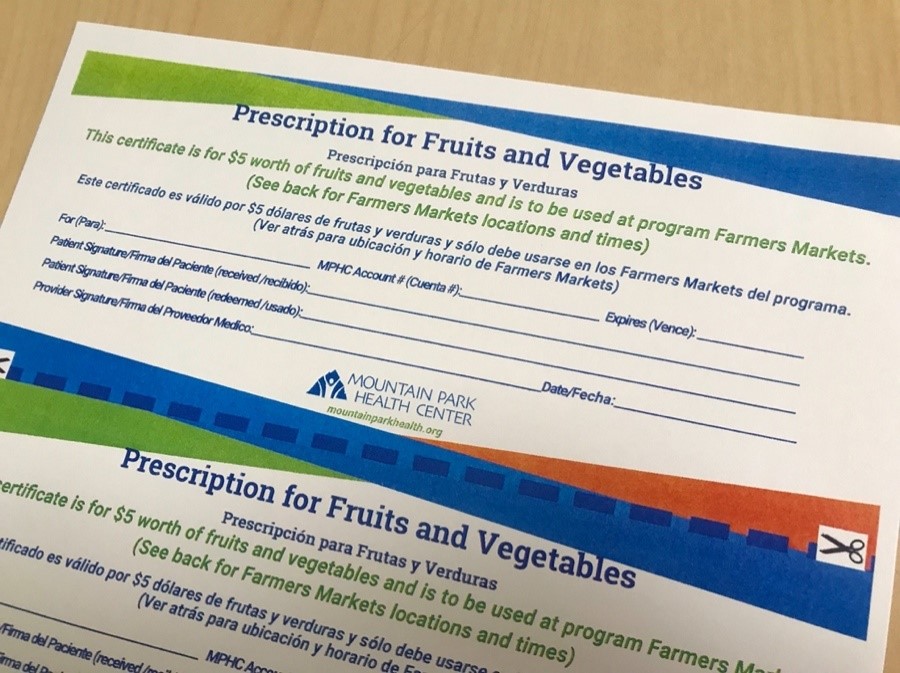
Through a small grant, Mountain Park began writing prescriptions for healthy foods that were distributed weekly at the diabetes self-management program. These prescriptions included a $15 voucher to be used at the farmers’ markets, along with recipe cards for that week’s available food. A local farmer also attends the program to explain what is available, and with a dietitian, they pre-package $5 bags of produce to make the buying experience even easier.
Southside Community Health Services, Inc. – Minneapolis, MN
To provide patients with strategies for managing diabetes, Southside partners with the University of Minnesota to host a six-week cooking course which includes general nutrition education, label reading, meal preparation, and a short exercise component. Participants are given the produce that they need to re-create the meal prepared during class at home. For one of the sessions, the class attendees go together to a grocery store to practice label reading and distinguishing between products. Patients who complete the full six-week course are gifted the individual hot plate that they used throughout the course.

In addition, Southside has established community gardens at two of its clinic sites. Participants in the cooking class visit the garden and receive its produce. The gardens are tended to by health center staff and community members alike. They also partner with a local food co-op to provide Community-Supported Agriculture (CSA) boxes. Diabetic patients and their families are prescribed the CSA boxes at no cost by the clinic’s providers, and the program runs for 16 weeks for 30 families at a time.
This article is part of the Diabetes Prevention Across the Lifespan Series, a 4-part article series published by MHP Salud and Health Outreach Partners.
Resources
HRSA Disclaimer
This webinar is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of awards as follow: Health Outreach Partners (HOP) National Training & Technical Assistance National Cooperative Agreement totaling $932,014.00 with 0 percent financed with non-governmental sources and MHP Salud National Training & Technical Assistance Cooperative Agreement totaling $753,959.00 with 0 percent financed with non-governmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS or the U.S. Government. For more information, visit www.HRSA.gov.
Citations
- https://www.cdc.gov/diabetes/managing/education.html
- https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/in-depth/diabetes-prevention/art-20047639
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3781525/pdf/2895.pdf
- https://www.cdc.gov/diabetes/ndep/pdfs/Food_Insecurity_Slides.pdf
- The USDA defines a food desert as “low-income tracts in which a substantial number or proportion of the population has low access to supermarkets or large grocery stores.” (https://www.ers.usda.gov/webdocs/publications/45014/30940_err140.pdf)
- These practices were sourced from HOP’s Innovative Outreach Practices report: Addressing Diabetes Through Outreach. June 2018. https://outreach-partners.org/2012/07/01/innovative-outreach-practices-report/
Blog Topics
About MHP Salud
MHP Salud has over 35 years of experience implementing CHW programs and training organizations looking to start and/or strengthen their own CHW programs. Visit our CHW Training & Consulting Services page to learn more about how we can help.