Migrant Seasonal Agricultural Workers and Latino Communities Managing Diabetes
Community Health Workers Addressing Cultural and Holistic Alternatives in Diabetes Management
Published June 2021 | Back to all news and updates.
Migrant Seasonal Agricultural Workers and Latino Communities Managing Diabetes
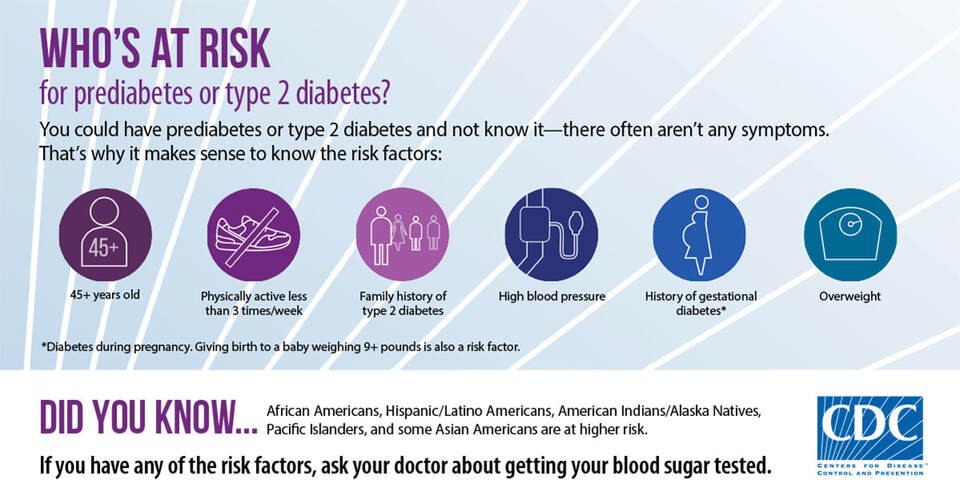
Migrant Seasonal Agricultural Workers (MSAW) are part of the underserved groups considered essential during the ongoing pandemic. More than 80 percent of MSAWs in the U.S. are Hispanic/Latino. Hispanic/Latino adults have a rate of about 50 percent of developing Diabetes Type 2 due to genetics, food, culture, weight, and activity. (1) MSAWs are more likely to have poor general health and limited finances. They often work long hours and may not be able to make their health a priority as they are trying to provide for their families. MSAWs and Latino communities are at higher risk of Type 2 diabetes; they may lack the education on how to manage this chronic illness. MSAWs travel for work often and may not know local resources in their different work communities. In addition, MSAWs may face other barriers to health such as lack of transportation, funds, healthy foods, or support to manage their diabetes. (1)
Health and Risk Factors of Migrant Seasonal Agricultural Worker Families
More than half of hired agricultural workers (51%) in the United States are of Hispanic/Latino descent placing them at higher risk of developing diabetes. (12) “Diabetes is known as one of the leading causes of death and disability in the U.S. alone and it is the fifth leading cause of death among Hispanics/Latinos in the United States” (2). Risk factors for Diabetes within the Latino community include being overweight, having a relative with diabetes (i.e., brother, sister, parents), being older than 45 years of age, and having a history of gestational diabetes. MSAWs do not visit doctors regularly and are more likely to have diabetes and not know it. (2) MSAWs are prone to the development of Type 2 Diabetes as adults due to various factors ranging from their work conditions, culture, genetics, and predispositions to include high-stress levels and long-term exposure to certain pesticides while working in the fields. (4)
Alternative/Holistic Medicine
MSAWs travel for work often and many do not attend regular doctors’ visits due to lack of health insurance, immigration status, language barriers, transportation, cultural beliefs, and/or distrust of services. MSAWs that do not speak English can face issues when explaining their symptoms to medical professionals. Information might be lost during translation, or MSAWs may not understand treatment instructions from their doctors. This can lead to confusion or distrust of doctors which ultimately affects MSAWs’ management of their diabetes. In the Latino community, it is common to use natural or traditional medicines for illnesses to replace standard medical treatments. These might include home remedies, traditional healers (i.e., spiritual healers, curanderos, sobadores, and herbalists), and other therapies. (1) Many people use various methods combining the use of traditional healers and medical care. In some instances, MSAWs will usually try home remedies for healing before seeing a medical doctor.
Cultural Beliefs
Cultural medicinal beliefs influence how MSAWs/Latinos make decisions about their health. In Latino culture, it is common to put the needs of the family before one’s own health needs; therefore, they may seek to try traditional medicines or treatments prior to spending money on costly medical visits, tests, or treatments. Because of the belief of not spending money on treating their condition or distrust of medical professionals, some MSAWs/Latinos self-medicate by purchasing medications from other countries at low cost and without a prescription to manage their diabetes and other health conditions. In some cultures, including Latino cultures, there are superstitions that if one talks about or voices a poor health outcome, it will occur. Because of this belief, some people might avoid seeing a doctor for their condition and might try other methods such as natural or spiritual healing. Natural and spiritual healing products can be found at local religious goods stores also known as botanicas which sell herbs, oils, candles, and soaps that are believed to help with certain medical conditions. (9)
Family plays a large role in making decisions on treatments and management; it can be challenging for the individual to make changes related to diet and exercise if these norms do not conform to the family unit. (8) This makes it difficult for someone in the household with diabetes to make changes to their diet to healthier options if there is lack of support from other household members to make diet changes as well. Being thin in the MSAW and Latino cultures is seen as being ill or unhealthy. Within this culture, celebrations are celebrated with high-calorie foods, and food is seen as a reward in some instances. The risk for diabetes increases in “obesogenic” environments where unhealthy food is inexpensive. (4) It is often more expensive to buy healthy foods which affects large families with limited incomes such as MSAW families.
Vaccine Confidence
MSAWs are essential workers and one of the first groups selected for vaccinations. Ensuring that MSAWs are vaccinated would secure the U.S. food supply and protect the workforce. (10) Besides their risk of crowded housing and working conditions, MSAWs are at higher risk of contracting COVID-19 complications due to their Diabetes. Since vaccines became available, the CDC has recommended that people with chronic medical conditions such as diabetes receive priority due to their increased risk of severe COVID-19-associated illness. (13) Although vaccines are now available, reservations on vaccines stem from a misunderstanding of vaccination costs and identification documents needed to receive the vaccine, locations for vaccines, and, most recently, fear of vaccine reactions as a cause of the Johnson and Johnson vaccine withdrawal. MSAWs depend on their daily incomes to feed their own families and missing a day or two from work to get vaccine dosages greatly affects their decisions to get the COVID-19 vaccine. MSAWs travel often due to their work and may not be in the same city, county, or state for the second dose; as a result, they may opt to forgo the vaccine. (11)
Studies have found that people with diabetes were 2 to 3 times more likely to be treated in the intensive care unit and/or die from COVID-19 in the hospital than people without the chronic illness. Vaccinations for Latinos are critical due to this community being disproportionately affected by both diabetes and COVID-19 leading to double the death rate of white Americans in 2020. (14) Due to their work, MSAWs live in isolated rural regions, far from testing, vaccination sites, and other resources. Having a member of their community, such as a CHW, who speaks their language and can answer any questions they may have can provide confidence in MSAWs with diabetes to receive COVID-19 vaccines. CHWs can provide resources and information to MSAWs in their preferred language to help them decide if vaccination is good for them (i.e., Assistance with vaccine registration, vaccine locations and hours and, health facts and/or side effects related to their diabetes with getting the vaccine).
Community Health Workers Addressing Diabetes
A CHW is a trusted member of the community they serve. CHWs work in both clinical and non-clinical settings and provide their community with resources to health and social services. CHWs meet participants where they are – at home, at work, or out in the community – to better reach participants and meet their unique needs. (5)
CHW roles can include cultural mediation, culturally appropriate education, care coordination, case management, systems’ navigation, coaching and social support, advocacy, capacity building, and outreach. Through these roles, CHWs offer support to patients with diabetes and/or at risk of developing diabetes in a unique culturally appropriate manner. Due to their close understanding of and trust from the community they serve, CHWs have a unique ability to build strong relationships and effectively address challenges individuals face when trying to manage chronic conditions such as diabetes. CHWs also conduct home visits and speak one-on-one with participants on the importance of proper nutrition, physical exercise, and disease management.5,6
CHW-led diabetes programs provide accessible support and education to vulnerable populations so they can live healthier lives. They focus on community-based educational classes led by a CHW and provide educational instruction on how participants can manage their diabetes and maintain a healthy lifestyle. CHWs can understand and culturally identify with the programs’ participants and provide appropriate recommendations that participants will be receptive to based on available resources and food options.6
Overall, CHW interventions have demonstrated success in improving health outcomes among individuals diagnosed with diabetes and support at-risk individuals to prevent the development of the condition. Although COVID-19 has challenged how many CHWs deliver services (i.e., telehealth or virtual), CHWs continue to find ways to engage their communities. At MHP Salud, our CHWs are using WhatsApp, Zoom, and other virtual tools to hold educational sessions. 5,6
Community Health Worker Testimonial

My name is Noelia Serrano and I have worked as a Community Health Worker for 18 years in various programs and agencies. The need I have seen in the community for health education on diabetes is big as many people are still misinformed on their diabetes condition and management. It is very hard to get participants to change their eating habits since, in our culture, we have been taught since we were small children to see food as a trophy for everything we do. For example, when kids do good in school we celebrate with food, every holiday we celebrate with food. We must reteach our minds to see the food as needed nutrients and not just something to satisfy our hunger. I have seen participants do the change and are having a better quality of life.
– Noelia Serrano, CHW for MHP Salud.
- https://www.cdc.gov/diabetes/library/features/hispanic-diabetes.html
- http://www.idph.state.il.us/idhp/idhp_HispanicRiskForDiabetes.htm
- https://www.southern7.org/diabetes-prevention.html
- http://www.ncfh.org/diabetes-fact-sheet.html
- https://mhpsalud.org/community-health-worker-resources/community-health-workers-diabetes/
- https://mhpsalud.org/programs/our-programs/juntos-podemos/
- https://scholar.google.com/scholar?q=Conventional+and+Complementary+Therapy+Use+among+Mexican+Farmworker&hl=en&as_sdt=0&as_vis=1&oi=scholart
- https://www.ahrq.gov/health-literacy/improve/precautions/tool10.html
- https://www.tampabay.com/news/health/2020/06/05/faith-in-herbal-remedies-fuels-growth-of-latino-botanicas-coronavirus-acclerates-it/
- Failing to vaccinate farmworkers exploits, endangers labor force (newswise.com)
- To Help Farmworkers Get COVID-19 Tests And Vaccine, Build Trust And A Safety Net : Shots – Health News : NPR
- https://agecon.ca.uky.edu/hired-farm-labor-and-the-role-of-hispanic-workers#:~:text=The%20observation%20about%20families%20providing,%25)%20of%20the%20national%20workforce.
- https://www.everydayhealth.com/type-2-diabetes/things-people-with-diabetes-must-know-about-the-covid-19-vaccines/
HRSA Disclaimer
This publication is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $753,959.00 with 0 percentage financed with non-governmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS or the U.S. Government. For more information, please visit www.HRSA.gov.
Blog Topics
About MHP Salud
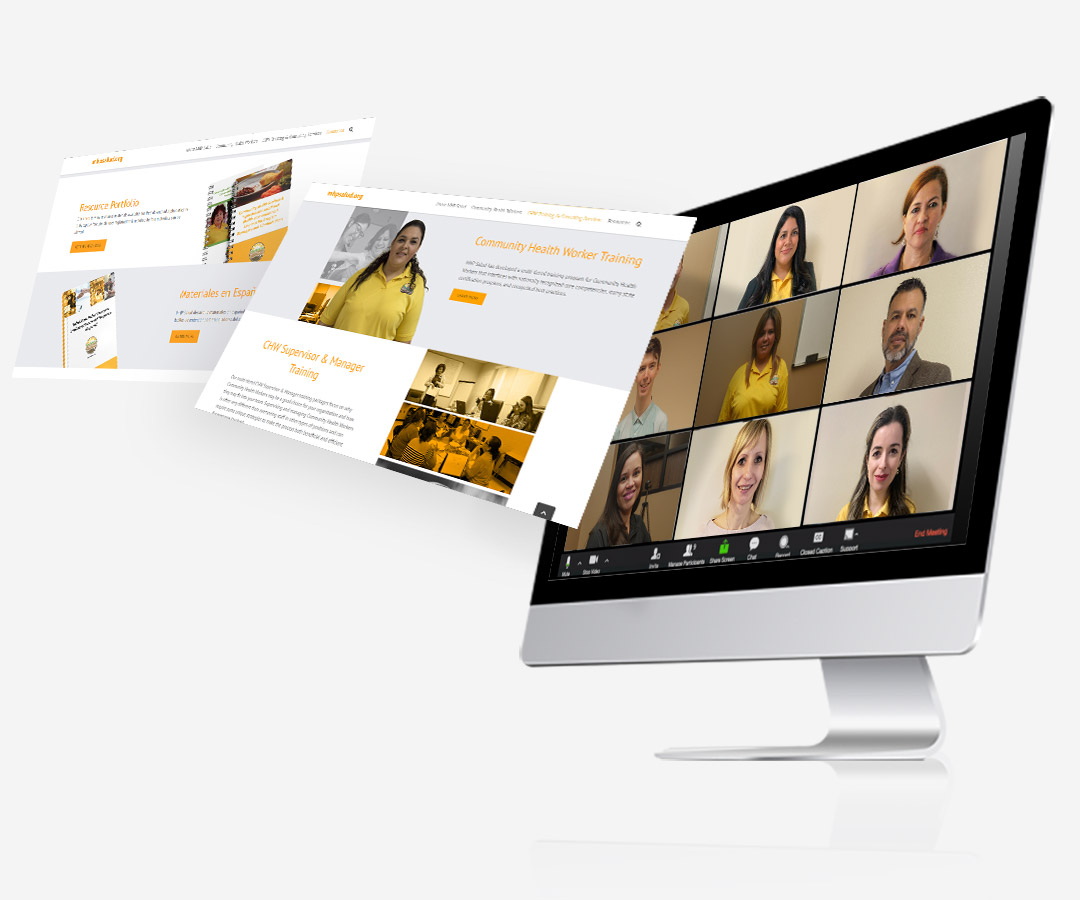
MHP Salud has over 35 years of experience implementing CHW programs and training organizations looking to start and/or strengthen their own CHW programs. Visit our CHW Training & Consulting Services page to learn more about how we can help.